III.1. Energy storage
The nutrition is controlled by various complex internal and external factors.
Since the 1970s, the gastrointestinal tract (GIT) has been recognized as playing a key role in the regulatory mechanisms.
The excess energy is stored as triglycerides (TG) in the adipose tissue. The TG are composed of one molecule of glycerol and three molecules of fatty acids.
The normal TG level < 3.9 mmol/l.
Under physiological conditions, the storage mechanisms (the biosynthesis of proteins from amino acids; TG from glycerol + free fatty acids (FFA); glycogen from Glu) prevail over the energy-releasing mechanism (from Glu) after eating (in the absorptive state, in the presence of insulin). After eating, the increased release of insulin enhances the replacement of a special Glu-transporter (type IV Glu transporter, GLUT-4) into the plasma membrane of the adipocytes, which increases the uptake of Glu from the blood. In the process of glycolysis glucose 3-phosphate is produced from Glu. Cholesterol is synthesized in the liver and in the small intestine, and is used for the synthesis of lipids. Lipoproteins are also important in the transport of FFA to the adipose tissue: the chylomicron (Chy) carries FFA absorbed in the small intestine, while the very low-density lipoproteins (VLDL) transport FFA synthesized or stored in the liver. The fatty acids are carried as TG by lipoproteins, but fatty acids in this form cannot be taken up by the adipocytes. The TG are digested to FFA and monoglycerides by the enzyme lipoprotein lipase (LPL), found on the surface of the capillaries. The activity of LPL is increased by insulin.
During the fasting phase (in the postabsorptive state, comprising in the lack of insulin), the catabolic pathways prevail, one possible source of energy comprising lipolysis, the catabolism of the TG.
In the adipocytes, the hydrolysis of TG requires lipases, the activities of which are increased by norepinephrine (N) released from the sympathetic nerves, by epinephrine (E) released from the adrenal glands, and by glucagon released from the pancreas. The released FFA bind to albumin and transport energy to various organs (e.g. the heart and the skeletal muscle). In the liver, the FFA are converted to ketone bodies, which are important energy sources especially for the brain (and also for the heart and muscles). Glycerol is converted to Glu (gluconeogenesis) primarily in the liver; Glu can serve as an energy source for many cell types. The fat deposits in the body help healthy humans to stay alive during a period of weeks fasting (Fig. 2).
Fig. 2. The effects of insulin on the mechanisms of energy storage
(in the absorptive state (in the presence of insulin) – blue arrow,
in the postabsorptive state (in the lack of insulin) – red arrow)
The five classes of lipoproteins based on their TG content:
- Chy
- role: transport of exogenous lipids
- content: cholesterol, TG, apolipoprotein B48 (ApoB48)
- size: the largest lipoproteins (>100 nm)
- VLDL - large lipoproteins
- role: transport of endogenous TG
- content: cholesterol, TGs, ApoB100, FFA
- size: 30-80 nm
- IDL – Intermediate density lipoproteins
- derived from the breakdown of Chy and VLDL
- size: 30-40 nm
- LDL - < 2.6 mmol/l
- derived from VLDL and IDL
- content: cholesterol, ApoB100
- types: LDL-A and LDL-B
- LDL-A larger, less harmful
- LDL-B a marker for many diseases, found in many patients with MetS
- size: 20-40 nm
- a lot of cholesterol and apo-A
- HDL (High Density Lipoproteins, small lipoproteins) - > 1.0 mmol/l
- derived from the catabolism of VLDL and Chy
- content: cholesterol, ApoB100
- size: the smallest, but the highest-density lipoproteins (5-12 nm)
- role: transport of cholesterol into the liver, inhibition of LDL oxidation and accumulation within the vessel wall.
Apo are proteins which are important in the structure and the regulation of lipoproteins (Fig. 3).
- Apo-A a component of HDL
- Apo-B a component of LDL and VLDL
- Apo-C involved in the regulation of LPL
- Apo-E the role of regulation
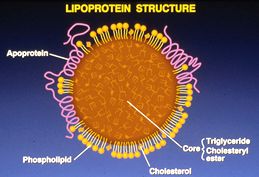
Figure 3. The structure of lipoproteins
(John R. Guyton: Basics of Lipid and Lipoprotein Metabolism (lipid clinic training program, National Lipid Association), Duke University, Durham, NC, USA)
The total cholesterol (TCH) is made of four components:
VLDL + LDL + IDL + HDL
Normal range: < 5.2 mmol/l
The ratio TCH/HDL is a marker of the risk of cardiovascular heart disease (CHD). A low level of HDL suggests a high risk of CHD.
The adipose tissue is the main source of FFA. The FFA level correlates closely with obesity and with an increased liver fat content. FFA contribute to the development of insulin resistance through inhibition of the insulin-related Glu uptake in the muscles and inhibition of the pancreatic beta-cells. The synthesis of fibrinogen and plasminogen activator inhibitor type-1 (PAI-1) is stimulated by FFA.
During eating, the adipose tissue is regulated by the sympathetic nervous system (SNS). SNS increases the immobilization of FFA. Epinephrine inhibits the insulin-stimulated uptake of Glu by the adipocytes, but has a stimulatory effect on the Glu uptake by the adipocytes in the lack of insulin. Catecholamines reduce the levels of Chy and VLDL through the inhibition of LPL, this enzyme catalyzing their production.
The daily energy expenditure of a healthy person:
60 % - basal metabolic rate
10 % - to maintain the body temperature
30 % - for physical activity
15-20 % of the energy is stored as fat (a higher percentage in women. A healthy, 70-kg man contains 15 kg of fat, 6 kg of protein and 0.4 kg of glycogen. The liver and the adipose tissue are the main and continuous energy sources. In the fasting state Glu is produced from glycogen in the liver, and in the adipose tissue TGs are hydrolyzed, releasing FFA (lipolysis).